Wheat, gluten, and mental health: Exploring the link
Original Article by Casey Means. Source
Anxiety and depression are rampant in America right now, with around a third of the population reporting an anxiety disorder and over 20% of adults having a major depressive episode in their lifetime. On top of this, chronic fatigue and brain fog are on the rise, and are linked to inflammation in the brain (a process called neuroinflammation). Hoards of scientific studies have suggested that diet and gut health have a profound impact on our mental health outcomes through the “gut-brain axis” as well as by the way in which our gut lining can protect our bodies from system-wide inflammation that can then trigger symptoms in the brain. A healthy gut lining and diverse microbiome serves as a strong barrier that limits the “outside world” from being able to overwhelm our bodies and cause problems (read an excerpt from Good Energyabout this, here).
The link is so strong between gut health and mental health that studies in animals have shown that just transferring the microbiome from depressed animals to healthy animalshas been shown to quickly induce depression-like behaviors!
In my own life, I have had two experiences where the gut-mood link has been strong for me. As I talk about in Good Energy, I had severe GI symptoms during my stress-filled, sleep deprived, cafeteria-fueled surgical residency when I was routinely working 100 hour weeks. Just a few months into surgical residency, I rapidly developed irritable bowel syndrome (IBS) where I had excruciating stomach pain and sometimes more than 10 episodes of diarrhea per day. Simultaneously, I developed life-crushing depression and anxiety. IBS and mental health issues are so linked that IBS is sometimes referred to as “depression of the gut,” and “treated” with tricyclic antidepressants.
Fortunately, 8-ish years later, my gut issues and depression are completely healed. In fact, these issues healed rapidly (within just a few months) after I quit my surgical residency and started living a more functional life again, with lots of whole colorful organic foods, regular sleep, sunshine, nature, movement, and less adrenaline-fueled days and nights in the operating room. During my issues with IBS, I kept a journal of my GI symptoms per the recommendation of my gastroenterologist at the time, and it’s hard to believe that person is me of the past… a person who had to pull over to the side of the highway because my abdominal pain and gas was so severe. (I’ll spare you any more details).
While I no longer have these severe symptoms, I do still have an issue where I notice swelling (i.e. in my fingers, where I can’t get my rings off) and anxiety soon after eating conventional wheat-containing products. It usually fades after a couple of days, but is noticeable to me. When I mentioned this symptom in a previous newsletter, I got an outpouring of interest around the relationship between wheat and anxiety. In this newsletter, I will share the science behind this fascinating link!
The modern destroyed gut
Our modern world is destroying our guts: both the lining of the gastrointestinal tract and a healthy microbiome diversity.
IBS, reflux, colorectal cancer, and inflammatory bowel diseases like Crohn’s and ulcerative colitis are rising significantly in recent decades.
What’s going on?
We know that there are many factors of our modern, stressed-out, sedentary, fast-paced convenience culture that are contributing. Some of the known culprits of damaged gastrointestinal function include:
- 🥤 Ultra-processed foods (UPFs): Industrially engineered ultra-processed foods (or “Frankenfoods” as I like to call them) make up the majority of our modern diets and often contain artificial additives, preservatives, synthetic flavors, emulsifiers, and pesticide residues, all of which can disrupt the gut microbiota and damage the gut lining.
- 🍫 Excessive sugar: High sugar consumption, particularly fructose, can promote the growth of harmful bacteria and yeast, leading to inflammation and compromised gut integrity.
- 😵💫 Chronic stress: psychological stress can alter gut microbiota composition and increase intestinal permeability by affecting the gut-brain axis. Chronic stress can come from many places: social media, unresolved childhood trauma and adverse childhood events, work, negative self-talk, caregiving responsibilities, relationships and more.
- 🤧 Overuse of antibiotics: Antibiotics can destroy the balance of gut microbiota and kill beneficial bacteria, weakening the gut barrier and causing inflammation.
- 💊 Frequent NSAID and anti-reflux use and overuse of medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and Aleve can cause intestinal inflammation and increase gut permeability. These are vastly overused in the modern world and have a significant impact on our gut. Many drugs impact gut function in bigger ways than we might imagine.
- 🫘 Low fiber and low polyphenol diet: Our microbiome bacteria ferment fiber and polyphenols to make healthful byproducts like short-chain fatty acids (SCFAs) that we absorb. A diet low in dietary fiber and polyphenols reduces the production of SCFAs which are essential for maintaining the gut barrier and key for metabolic health. Polyphenols are natural chemicals found in colorful fruits, vegetables, nuts, and spices that are exceedingly good for our microbiome.
- 🍞 Gluten consumption: Gluten can trigger the release of zonulin, a protein that increases intestinal permeability. You’ll read more about this below.
- 🍸️ Alcohol consumption: Alcohol can cause inflammation of the gut lining and disrupt the tight junctions between intestinal cells, leading to increased permeability.
- 😴 Poor sleep: Lack of sleep or poor sleep quality and irregular Circadian signals triggers stress hormone release and can disrupt the gut microbiota and negatively affect the gut barrier.
- 🚶♂️ Not moving enough: Physical inactivity has been associated with unfavorable changes in gut microbiota composition and increased intestinal permeability. Exercise is incredibly protective for a healthy microbiome composition.
- 🔥 Chronic inflammation: Chronic low-grade inflammation, often resulting from obesity, metabolic syndrome, environmental toxins, stress, and many other factors, hurts the gut lining, because inflammation is a form of “battle” in the body that has significant collateral damage on our bodies.
- 🍬 Artificial sweeteners: Some artificial sweeteners like aspartame and sucralose can negatively impact gut microbiota and contribute to gut barrier dysfunction.
- ⚠️ Environmental toxins: exposure to environmental toxins like heavy metals, pesticides, air pollutants, and more can damage the gut lining and microbiome compositing and contribute to increased permeability.
- 😎 Vitamin D deficiency: Vitamin D plays a role in maintaining gut barrier integrity. Many Americans are low in vitamin D. We want to be at least in the 40-60 mg/mL range.
- 🐟️ Low omega-3 fat intake: Omega-3 fatty acids have anti-inflammatory properties and support gut barrier health.
- 🦠 Infection: Bacterial and viral infections can both distort our microbiome and gut lining, including COVID-19.
- ☀️ Not enough sunlight: research has shown that populations who are not exposed to adequate sunlight have less favorable microbiome profiles. The average American is now indoors or in a car 93% of the day.
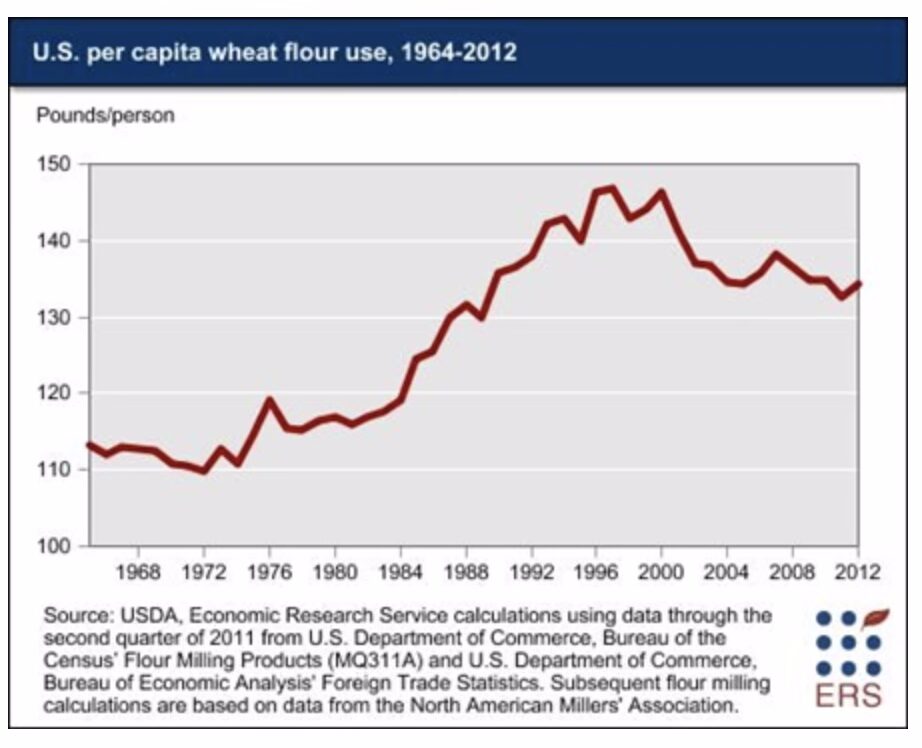
On top of this, the quality of our diets have shifted massively in the last 100 years. For starters, we are eating an astronomical amount of wheat flour, much more so than in the 1960s:
So, is wheat causing mental health issues like anxiety and depression?
It’s definitely not that simple.
What is more likely occurring is that there is a persistent, daily attack on the microbiome and gut lining from the 17 factors listed above (and many more) creating a gastrointestinal (GI) tract that is more susceptible to negative effects of the vast amount of conventional, ultra-processed, high-gluten wheat we are eating today. Wheat contains proteins that can impair several elements of gut function, and in combination with the multitude of other environmental factors hurting the gut lining and microbiome, we get systemic inflammation that affects the whole body, including the brain. We’ll discuss all of this, below.
The spectrum of gluten-related disorders
Wheat is a type of grain, and it is one of the three foods that make up 50% of the world’s caloric intake in modern times (rice, wheat, and corn). Wheat contains many proteins and molecules, including gluten (which contains gliadin and glutenin proteins), amylase-trypsin inhibitor proteins (ATIs), and others. While wheat has long been a staple in the human diet, it seems that wheat-related disorders are on the rise.
In individuals with celiac disease, which affects approximately 2 million people in the United States, this immune response to gluten is severe, leading to inflammation and damage to the intestine. Some data suggests that celiac disease is rising at a rate of 7.5% per year 😱. However, even in non-celiac individuals, wheat proteins can affect gut integrity through several mechanisms.
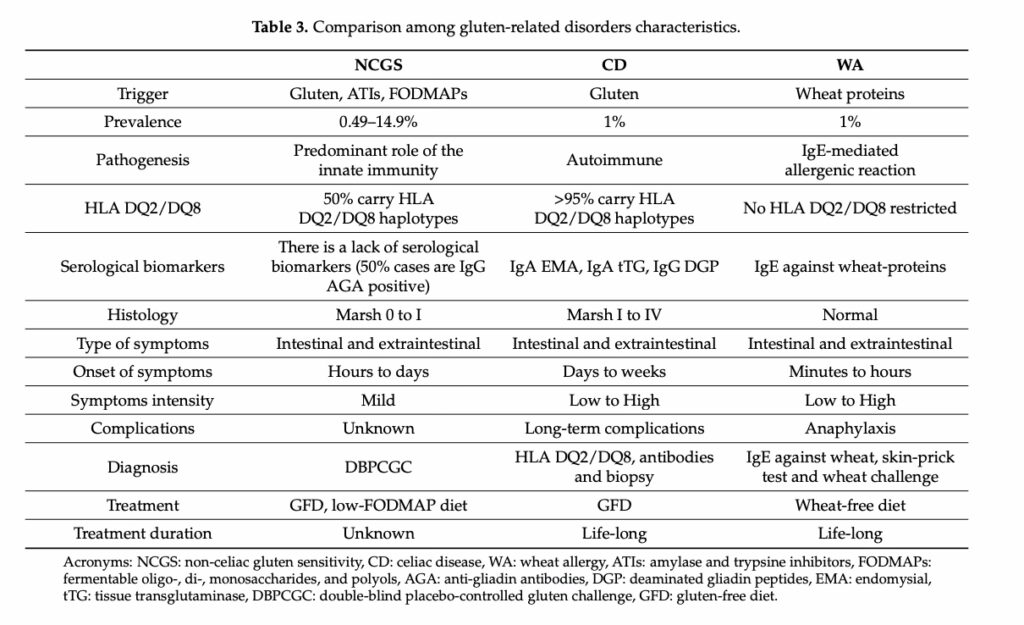
Non-celiac gluten sensitivity, or more broadly, non-celiac wheat sensitivity (NCWS) affects up to 15% of the population and is defined as “a syndrome characterized by intestinal and extraintestinal symptoms related to the ingestion of gluten-containing food, in subjects that are not affected by either Celiac Disease or Wheat Allergy.” The symptoms are “gastrointestinal symptoms are bloating, abdominal pain, diarrhea, nausea and reflux. The extraintestinal manifestations are widely heterogeneous and include headache, general tiredness, blurred mind, fibromyalgia, lack of well-being, dermatitis, joint pain and depression.”
There is also a clinical category of “Wheat Allergy,” which affects about 1% of the population and is a true allergic reaction (IgE mediated reaction) to wheat proteins.
You can see a summary of these conditions, below:
Gluten, zonulin, intestinal permeability, and inflammation
To understand how problems in the gut can lead to problems in the whole body, we need to understand the concept of “intestinal permeability.” The gut epithelium (aka, gut lining) is composed of tightly packed cells held together by structures known as tight junctions, which are like little anchors between cells that keep the gut lining impermeable and strong. These tight junctions regulate the passage of substances between the tube of the gut (where food passes through) and the bloodstream, maintaining the selective permeability of the intestinal barrier so only certain things can get through from the inside of the gut into the body and bloodstream.
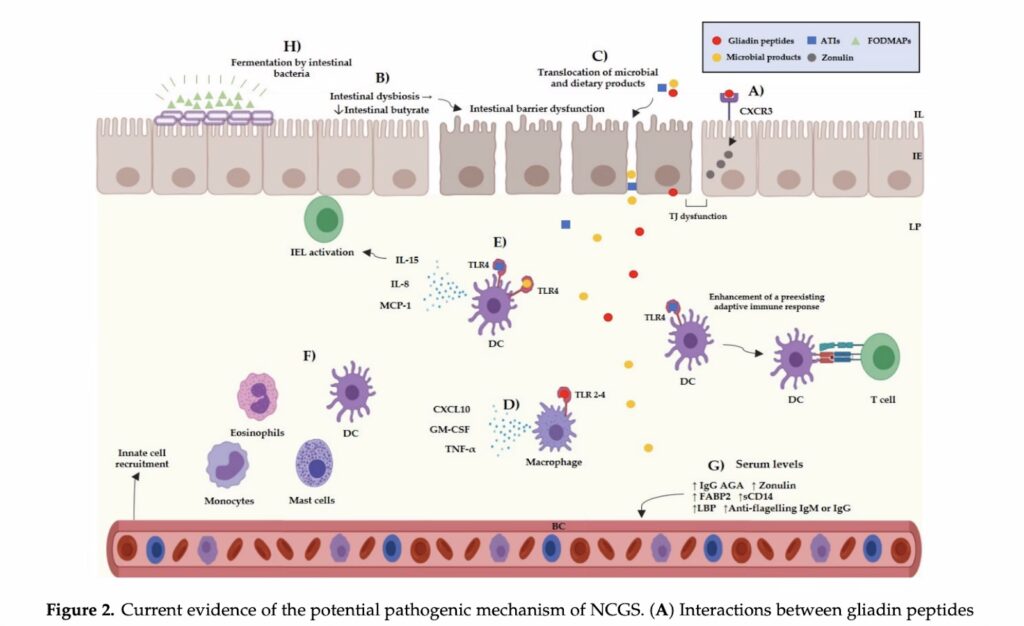
Zonulin is a protein that is a key regulator of these tight junctions. When zonulin is upregulated (increased), it causes the tight junctions to loosen, increasing intestinal permeability—a condition often referred to as “leaky gut.”
Research has shown that gliadin, a component of gluten, can stimulate the release of zonulin in both celiac and non-celiac individuals. This gliadin-induced zonulin release leads to a temporary increase in intestinal permeability, allowing larger molecules, such as partially digested food particles, toxins, and pathogens from the gut to enter the bloodstream, where they are NOT supposed to be.
This breach of the intestinal barrier can then initiate systemic inflammation, as the inside of the body is not “used” to seeing these molecules that are supposed to be in the gut, and views them as foreign and potentially dangerous (therefore inciting inflammation). Chronic inflammation has been implicated in various chronic conditions, including autoimmune diseases, metabolic dysfunction, and mental health disorders.
If there is a “war” being waged by your immune system in your body (aka, chronic inflammation), it makes sense that it would have an impact and lead to symptoms. You can see this war being kicked off in the image from this paper, below:
Systemic inflammation and mental illness
The “gut-brain” axis refers to the bidirectional communication between the gastrointestinal tract and the brain and spinal cord, or the central nervous system (CNS). This communication occurs through neural, hormonal, and immune pathways.
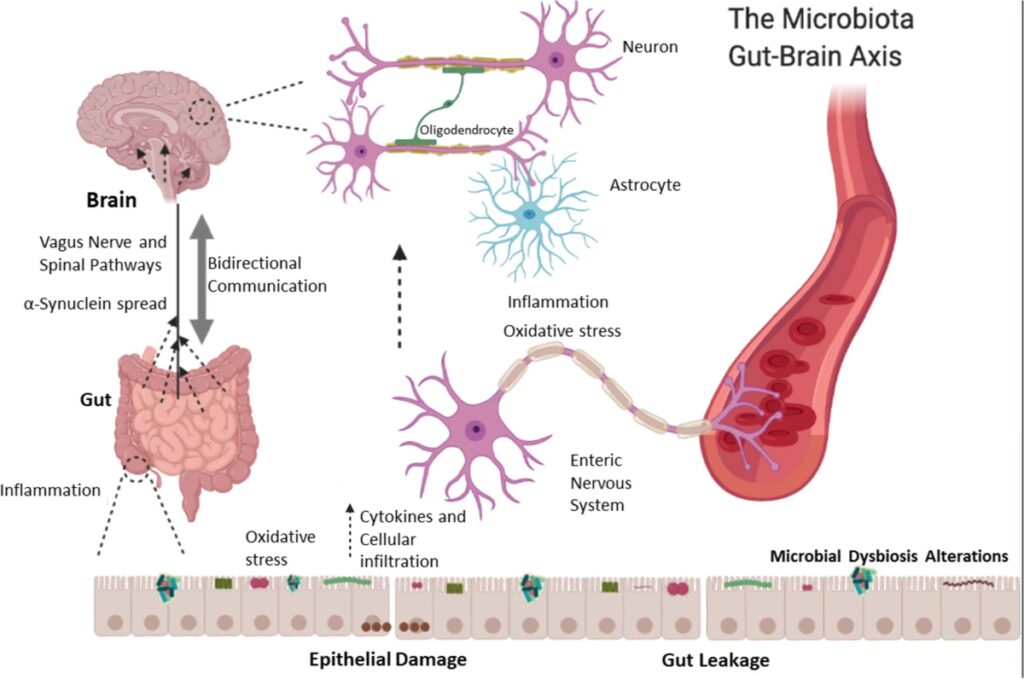
When the integrity of the intestinal barrier is compromised due to increased permeability, systemic (full body) inflammation can ensue. This inflammation is characterized by the release of pro-inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-α), interleukin-6 (IL-6), and interferon-gamma (IFN-γ). These cytokines can cross the blood-brain barrier (BBB) and induce neuroinflammation, affecting brain function and contributing to the development of anxiety and other mood disorders.
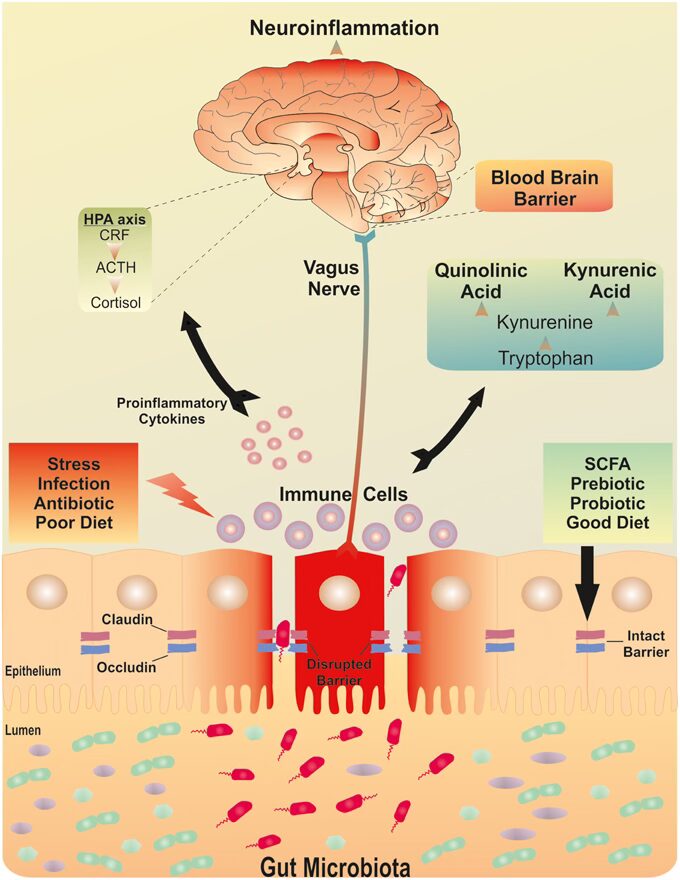
Research has demonstrated that chronic low-grade inflammation is associated with alterations in neurotransmitter systems, particularly the serotonergic (serotonin) and glutamatergic (glutamate) systems, which are crucial for mood regulation. For instance, inflammatory chemical IL-6 has been shown to reduce the availability of tryptophan, the precursor to serotonin, leading to decreased serotonin production. This reduction in serotonin, often termed the “feel-good” neurotransmitter, is linked to the onset of anxiety and depression.
For people with Celiac disease, depression, anxiety, and fatigue are more common than in the general population. This makes sense: the gut-brain axis strongly influences our mental health.
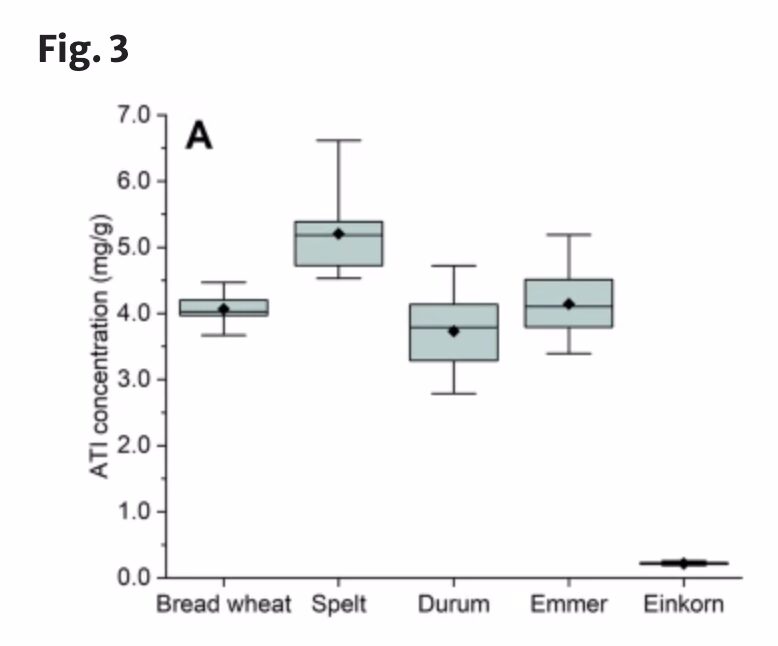
Amylase-trypsin inhibitors (ATIs) – a non-gluten wheat trigger of inflammation
In wheat, amylase-trypsin inhibitors (ATIs) are a class of proteins that serve as a natural defense mechanism for the plant, protecting the wheat from pests and pathogens. These proteins inhibit enzymes in the digestive systems of insects and microorganisms, helping the plant survive by deterring consumption and infection. ATIs can trigger immune responses by stimulating immune cells in the human gut, as well. Unlike gluten, which primarily affects individuals with celiac disease or gluten sensitivity, ATIs can provoke inflammation in a broader range of people, potentially impacting gut health and contributing to issues like intestinal inflammation and worsening of autoimmune conditions. Certain types of ancient wheat (like Einkorn wheat) appear to have significantly less ATI content than conventional wheat – here are two varieties (first, second) of organic Einkorn wheat I might give a try (haven’t yet tried so I can’t report!).
DPP-4: an enzyme that helps break down gluten implicated in mental health
DPP-4 is an enzyme that regulates glucose metabolism by breaking down certain hormones (like GLP-), which are involved in insulin secretion and blood sugar control, and it also plays a role in immune function. DPP-4 is widely expressed throughout the body, especially in the liver, kidneys, intestines, and immune cells. Of its many roles, DPP-4 is involved in the digestion and breakdown of gluten. In people with low DPP-4 levels or activity, it may impact the ability to fully degrade gluten peptides during digestion, allowing these peptides to enter the bloodstream and trigger immune responses or intestinal inflammation.
Gliadorphin (also known as gluteomorphin) is an opioid peptide that is formed during digestion of the gliadin component of the gluten protein. According to Board certified psychiatrist James Greenblatt, MD, “elevated levels of gliadorphin have been found consistently in patients with schizophrenia, autism, attention-deficit-hyperactivity disorder, depression, and other psychiatric illnesses. Abnormally low activity of DPP-4, involved in the breakdown of gluten, offers a potential link…When gliadorphin is not broken down by DPP-4, neurotoxic levels accumulate and produce psychoactive effects.”
He adds, “patients with elevated urinary gliadorphin also demonstrate clinical behavioral improvements when gluten is removed from the diet…DPP-4 also behaves as an immunomodulator, inducing the activation and proliferation of certain immune cells, providing an additional mechanistic explanation for the excessive inflammation seen in both celiac disease and mental health disorders…Finally, normal DPP-4 activity depends on adequate levels of zinc and other nutrients, which are commonly deficient as a result of poor intestinal function.” Studies show that more anxiety symptoms in children are associated with lower circulating levels of DPP-4.
So, DPP-4 and its activity may be another piece of the puzzle in understanding the relationship bewteen gluten and mental health. But it may be more complicated than it seems. DPP-4 inhibitor drugs are used for type 2 diabetes treatment (in part because these drugs increase GLP-1 levels), and some evidence suggests these meds improve depression. This seems to contradict the notion that lower DPP-4 levels lead to mental health issues, and is an area I want to dig into more.
Anxiety as a symptom of gut dysfunction
Anxiety is a complex and multifactorial disorder, with both genetic and environmental factors playing a role. However, the link between gut health and anxiety has become increasingly evident. Studies have shown that individuals with anxiety disorders often exhibit altered gut microbiota, increased intestinal permeability, and elevated levels of systemic inflammation.
Research has found that patients with anxiety had significantly higher levels of zonulin, suggesting that increased intestinal permeability may be a contributing factor to anxiety. Moreover, gluten-free diets have been shown to reduce symptoms of anxiety and depression in small studies in people with non-celiac gluten sensitivity.
As is summarized in Zonulin as a Potential Therapeutic Target in Microbiota-Gut-Brain Axis Disorders, “the spread of gut-derived microbial fragments, toxins, and inflammatory factors, including zonulin, finally reach distant organs, including the central nervous system, leading to increased blood–brain barrier (BBB) permeability, neuroinflammation, and behavioral changes… All these together suggest that dysbiosis and the zonulin pathway may be central factors in microbiota–gut–brain axis-related diseases.” Simply put, leaky gut may be leading to “leaky brain.”
Modern wheat is very different from the past
The widespread use of glyphosate, a herbicide, has been shown to disrupt gut microbiota, further compromising gut health. The combination of higher wheat intake, altered gut microbiota, and a damaged gut lining are likely exacerbating the effects of gluten on intestinal permeability and systemic inflammation.
Moreover, modern gluten-containing foods often contain added sugars, preservatives, and emulsifiers, which can further disrupt gut microbiota and contribute to intestinal permeability. A study in mice highlighted the role of emulsifiers in promoting low-grade inflammation and metabolic syndrome by altering the gut microbiota and increasing gut permeability. This synergistic effect of gluten and other damaging dietary components can have profound implications for gut health and, consequently, mental health.
Read more here: Why Modern Wheat Is Making Us Sick | Chelsea Green Publishing
Wrapping it up
The relationship between wheat proteins, gut dysfunction, and mental health symptoms is a complex interplay of dietary and lifestyle factors, intestinal permeability, systemic inflammation, and brain function. Wheat containing foods have high levels of several molecules like gluten and ATIs, and coupled with widespread impaired gut function in the modern world, this may promote neurologic symptoms via their impact on triggering systemic inflammation.
💕 13 ways to support the microbiome and gut lining:
- 🫘 Consume a fiber-rich and polyphenol-rich diet: Give the microbiome food it wants! This includes prebiotic fibers and polyphenols from foods like beans, lentils, berries, vegetables, nuts, seeds, and spices.
- 🦠 Eat lots of fermented foods: Unsweetened yogurt, kefir, sauerkraut, kimchi, beet kvass, and miso in your diet to seed the microbiome with live active probiotics.
- 😰 Prioritize getting on top of stress: Chronic stress can negatively impact gut health. Practices like meditation, yoga, deep breathing exercises, and spending time in nature can help reduce stress and support gut function. Identify stress triggers in your life like social media, toxic relationships, and negative thought patterns and work to set barriers with them.
- 🙅🥤 Eliminate ultra-processed foods and ultra-refined sugars: Ultra-processed foods and added sugars destroy the gut. Commit today to getting rid of them.
- 🏃 Move much more: Physical activity directly promotes healthy digestion and positively influences gut microbiota composition. Americans aren’t getting nearly enough movement; we’re meant to be moving almost all day. Aim for regular, moderate movement throughout the day (at least 10,000 steps! Read Good Energyfor the reasons why), and resistance training at least 2 days per week.
- 😴 Sleep: Quality sleep is crucial for overall health, including gut health. Poor sleep can disrupt gut microbiota balance. Aim for 7-9 hours of sleep per night, ideally uninterrupted and in a very dark room.
- 💊 Avoid overuse of antibiotics: Antibiotics can deplete beneficial gut bacteria, so they should be used only when necessary. They should be used when medically necessary, but not indiscriminately.
- 🦥 Incorporate mindful eating: Eat slowly, chew thoroughly, and pay attention to hunger and fullness cues. This can help with release of digestive enzymes and support gut motility.
- 💊 Consider supplementation: Consider supplements like probiotics, prebiotics, digestive enzymes (you can even find some digestive enzymes with DPP-4), or specific nutrients like L-glutamine and zinc, vitamin C and D, that support gut lining health. Consult with a healthcare provider before starting any new supplement.
- 🥦 Choose organic, and ideally regenerative, foods: Whenever possible, opt for organic food, which are grown without synthetic pesticides and herbicides. Read more about regenerative agriculture here: Why the way our food is grown matters for metabolic health.
- 👩🌾 Interact with organic soil: Gardening and getting our hands dirty in organic soil is beneficial because it helps expose our bodies to more diverse healthy microbes (and is good for the soul!).
- ☀️ Get MUCH MORE sunlight: Circadian biology and vitamin D are critical for health gut composition. We are not getting NEARLY enough sunlight in our modern lives, with 93% of our time indoors. Trying to spend several hours outside each day at a minimum. Read more about how to do this here.
- 🌾 Choose less inflammatory grains: If you’re going to eat wheat, consider ancient varieties like Einkorn. Also, choose only organic varieties, and ideally whole-grain forms, instead of ultra-processed.
